From the archives: A Story of 20,000 Healthy Mothers and Babies by Dr. Nosakhare Orobaton
[Originally published as a PLOS BLOGS Network guest post on December 10, 2013]
By Dr. Nosakhare Orobaton

To mark Year Three of the Maternal Health Task Force (MHTF) Collection, PLOS BLOGS Network is re-publishing an extraordinary pair of posts (edited for length here) by Dr. Nosakhare Orobaton, a MHTF collection author, physician and 30-year global health program administrator.
In his research article (coauthored with Bolanji M Fapohunda) “When Women Deliver with No One Present in Nigeria: Who, What, Where and So What?, contained in Year Two of the MHTF PLOS Collection, Dr. Orobaton provides an overview of contributing causes behind Nigeria’s continuing high maternal mortality rate.
In the blog post that follows (edited from the two previously-published posts), Dr. Orobaton chronicles a promising global health program aimed at improving the resources and conditions for maternal and newborn survival in his home country.
–V. Costello, PLOS BLOGS Network
April 22, 2013; Gagi suburb of Sokoto town, Nigeria

On this Sunday night, the starless, breezeless sky is pregnant with rain clouds and aglow with a waxing moon. The temperature is slightly less than the 45 degrees Celsius which held sway much of the day.
The community of Gagi is in transition. Old mud houses are slowly giving way to those built with cement blocks, a sign of growing prosperity. The scatterings of neem trees appear to affirm the community’s unyielding resilience and resolve to challenge the insatiable embrace of the ever-expanding frontiers of the Sahara Desert. It also hints to a touch of community defiance to outside forces, for better or for worse. Much of Gagi is quiet by night. But in a house 300 meters off the main road, this silence is broken by the piercing, heartwarming first cry of a newborn baby.
For now, it goes by the name Baby Nasiru.
It is here in Gagi that public health history is made for Nigeria; and Sub-Saharan Africa. Baby Nasiru is the first newborn to benefit from the Sokoto State government-sponsored community-based distribution programme to deliver to every child, Chlorhexidine 4% gel. This simple application prevents cord infection, a cause of one in three neonatal deaths in Nigeria. Also as a part of this program, Baby Nasiru’s mother Suwaiba receives and ingests Misoprostol tablets to prevent bleeding associated with childbirth.
Much of the country’s aspirations now ride on the expectation that such history making events will mark the beginning of the end of a world of indefensible and avoidable deaths of neonates in their first month of life; as well as the death of mothers during the seven million annually occurring childbirths in Nigeria.
Father: Nasiru
Nasiru is the man of the house, the husband of Suwaiba and father of the newborn. He is an unabashed tinkerer and a self-taught electronics engineer. He makes his living cobbling working TVs out of carcasses of abandoned TV sets that presently form a rising three-foot high pyramid on his lot. His electronics laboratory which doubles as his showroom is located in the front of his cement house, which opens into the street. Armed with secondary education, and his deep faith in the practice of Islam, Nasiru passionately brings the world to the community through the television. His showroom is also adjacent to the private rooms and courtyard where Suwaiba, his newest and second wife, is confined to a life of purdah.
Mother: Suwaiba
Suwaiba reads and writes Arabic; her education limited to Koranic school. She does not leave the compound. She does not go to the market. Suwaiba has never attended a clinic for prenatal visits, although she has delivered babies five times since she got married at the age of 16 years. Suwaiba is 25 years old. She has never delivered a child in a health facility. Her one source of information is what Nasiru tells her. Another is word of mouth brought in by other women, whom Nasiru approves of. No one can get to Suwaiba without his consent. Similarly, Suwaiba cannot reach out to people and institutions outside her home without Nasiru’s express consent.
When Suwaiba went into labor, she did not go to the nearby health center that was recently upgraded with support from the state and Federal Governments and their partners. It is unlikely she even asked to go to the health center.
Community Health Volunteer: Halima
On this night, Suwaiba’s husband contacted Halima, the local traditional birth attendant, and trusted woman in the community, who also doubles as a community-based health volunteer. Halima is one of the over 2000 trained community health volunteers in the state. Ten of them are in Gagi. Sokoto State government and USAID worked in tandem to train these volunteers who are now a vital source of information to women and men in communities across Sokoto state. In the last three months alone, largely as a result of these volunteers’ efforts, the average number of prenatal visits per woman has doubled from one to two. Halima is a critical part of the health system that makes the household level distribution of knowledge, information and medicines possible. She is also a fountain for the nurturing and growth of local trust, the oxygen of this program.
On this night, Halima contacted a community designated and trained drug keeper who dispenses medicines when labor is confirmed to have begun. Less than 1,000 minutes later, on Monday morning, Suwaiba and Nisuru’s son is safely delivered, just before the call to Fajr prayers. It is Suwaiba’s fifth delivery, and this one produces her first son.
Medicines: Misoprotol, Chlorhexidine 4% gel
Halima took the delivery of the baby, gave Suwaiba the recommended three tablets of Misoprostol to swallow, cut the umbilical cord with a clean razor, tied the cord appropriately, applied Chlorhexidine on the cord stump and delivered the placenta.
Nasiru allowed information about these two life-saving medicines to penetrate his household. He agreed for the medicines to be used for his wife. He also has consented for his son to be immunized. He did not have to. Yet, he did. It is the spirit of the tinkerer at work. Consenting parents need the backing and support of state governments to ensure that these low cost, high impact lifesaving medicines are available on a predictable basis.
It is the first time that these medicines are being offered to all political wards in a state, in any state in Nigeria, or elsewhere in Africa. It is also the first time that Chlorhexidine 4% is being used for cord care at population level. Only Nepal has a more developed programme. Government statistics estimate that in Sokoto State alone, with the introduction of Chlorhexidine, the programme would save 2,000 newborns from death in the first month of life each year. When applied across Nigeria, 60,000 deaths could be averted. In the case of Misoprostol, 1,000 women will be saved from dying each year in Sokoto State and 10,000 women nationally.
Baby Nasiru was brought out to meet visitors when he turned 5 days old. He appeared very healthy and active. His cord stump was dry and clean. In a few days, he will be seven days old. He will get his own name. Suwaiba did not reveal it.
“I thank the Almighty and the government for making this program available. It must be continued for all other women,” she said. Nasiru agreed. There was no need to tinker with what they now know works. A new dawn may well have arrived. What remained was to sustain it through the power of governance.
September, 2013:
On the morning we met Baby Rukayatu in Zangalawa village, 30 minutes from Sokoto Town in north-western Nigeria, the desert sky was blue and visibility was as good as it gets. The ground, still soaking wet from a recent downpour, hosted a riotous festival of flowers and vast armies of towering, green stalks of millet in bloom. The quiet slumber around the village was periodically awakened by the chatter of young children, the bleat of goat kids and by the sound of mortars pounding.
Father: Mohammed
Wrapped in royal purple cloth in the arms of her father, Mohammed, Rukayatu’s navel was strikingly clean and well healed. At birth, two weeks earlier, she had had the antiseptic gel , Chlorhexidine 4% applied to her freshly cut umbilical cord stump. Rukayatu’s mother also received inexpensive Misoprostol tablets, to prevent postpartum bleeding, which causes 25% of maternal deaths in Nigeria.
Said Rukayatu’s father, “I have to be frank. I did not at first care for these medicines. When I informed the dispensary health assistant that my wife had just delivered a baby, he really encouraged me to try them for my wife, and for my girl. Now, I am happy he convinced me to use them.”
Community Health Volunteer: Hawau
An elderly community health volunteer and long-time traditional birth attendant, Hawau supplied the medicines to Rukayatu’s father. Less than five feet tall and clad in a long blue print cloth and a marigold scarf that doubled as a hijab, her breakout smile outshined the old smallpox scars on her face. The multi-sized callouses on her hands hinted at a life of struggle and survival. “These medicines are a lot of help,” she said. “The assistance needs to be continued.”
Hawau collected her supply of these medicines from Mallam Tudu Abakar, who was appointed by the community to be their drug keeper on 24-hour duty. “These two medicines are miraculous,” Mallam Tudu said. “As drug keeper, I can tell you that the first stock of medicines I received from the dispensary is used up. I am now on my third batch. The government needs to realize that this program is important to us. It is working to save the lives of babies and mothers. It is important for this program to continue.”
Rukayatu is the 20,000th baby to receive Chlorhexidine 4% gel since late April of this year.
The Community and the Program
Sarkin Garba Bagarawa, the tall, regal-looking district head of Kwacar Lalle, spoke to us in his palace.
“We were consulted on this program at every step of the way. We nominated community health volunteers and drug keepers to be trained. We also know what is going on. We believe in it.”
This intervention, which could cut neonatal deaths by as much as 18 to 23 percent, was realized through Africa’s largest, ongoing community-based distribution program at scale, financed by Sokoto State government with support from USAID and a consortium of organizations led by John Snow, Inc. Sokoto’s approach to scale-up is quite novel because it leverages prior and ongoing improvements in the health system; it also encourages managers to adjust the program in real time with learning supplied by experience.
In this program, what good governance has initiated, trust-based community ownership has so far maintained. That such a program is rapidly producing remarkable results in an environment as imbued with the nuances of culture, socio-economics, gender and power relations as this one, is a testimonial to what is possible elsewhere in the country.
With approximately 5 million births every year in Nigeria, the journey that has begun in Sokoto needs nurturing, and be adopted by other state governors. As Nigeria and the global community dwell on progress towards to the UN 2015 Millennium Development Goals, we would all benefit from lessons learned here. The federal and 36 state governments in Nigeria will do well to ensure the timely supply of these medicines to satisfy the increasing demands of communities for the safe delivery of babies and their mothers. A little governance for tots will count for lots of tots’ lives saved.
This post was originally published in two parts at Weekly Trust, Healthy Newborns Network, and on the Gates Foundation Impatient Optimists blog , as “Good Governance and Protecting Newborns in Sokeko.” The Maternal Health Task Force at Harvard School of Public Health receives funding from the Bill & Melinda Gates Foundation. (http://www.gatesfoundation.org/)
A complete table of contents for all papers contained in Year Two of The Maternal Health Task Force (MHTF) – PLOS Collection, with the theme “Maternal Health is Women’s Health” (2012-13) can be found here.
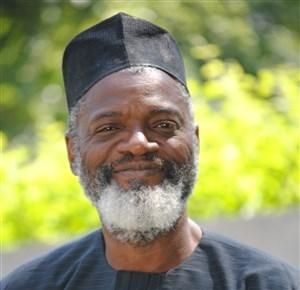 Dr. Nosakhare Orobaton (@nosaorobaton) is a public health physician with a background in business management. He is a Senior Advisor on Global Health for John Snow, Inc. Currently, he serves as the Chief of Party, USAID/Nigeria Targeted States High Impact Project (TSHIP), JSI Research & Training Institute, Inc. Dr. Orobaton worked for WHO in Geneva, Switzerland from 2007-2011, where he served as Deputy Executive Secretary. From 2006-2007, Dr. Orobaton was Director of Operations for The Global Fund to Fight AIDS, TB and Malaria, and managed a $ 7.5 billion portfolio of grants to 145 countries. He is currently spearheading the introduction, use and the local manufacture of Chlorhexdine 4% gel in Nigeria, for the prevention of cord infection in newborns. Dr. Orobaton is a member of the Technical Advisory Group of the Routine Health Information Network (RHINO) and the Global Chlorhexidine Working Group.
Dr. Nosakhare Orobaton (@nosaorobaton) is a public health physician with a background in business management. He is a Senior Advisor on Global Health for John Snow, Inc. Currently, he serves as the Chief of Party, USAID/Nigeria Targeted States High Impact Project (TSHIP), JSI Research & Training Institute, Inc. Dr. Orobaton worked for WHO in Geneva, Switzerland from 2007-2011, where he served as Deputy Executive Secretary. From 2006-2007, Dr. Orobaton was Director of Operations for The Global Fund to Fight AIDS, TB and Malaria, and managed a $ 7.5 billion portfolio of grants to 145 countries. He is currently spearheading the introduction, use and the local manufacture of Chlorhexdine 4% gel in Nigeria, for the prevention of cord infection in newborns. Dr. Orobaton is a member of the Technical Advisory Group of the Routine Health Information Network (RHINO) and the Global Chlorhexidine Working Group.


[…] A Story of 20000 Healthy Mothers and Babies: Announcing Year Three of the …PLoS Blogs (blog) In the blog post that follows (edited from the two previously-published posts), Dr. Orobaton chronicles a promising global health program aimed at improving the resources and conditions for maternal and newborn survival in his home country. Dr …and more […]
Congratulation to the team of Dr. Orobaton, who had successfully improved the resources and condition of maternal health in Nigeria. We all know that having babies in developing nations may be life threatening because of avoidable complications such as contamination of umbilical cord stump. Public health research was able to help Nigeria produce reliable and accurate documentation to inform the many critical decisions and actions that must be made about health systems. We hope that the hard-work will continue to produce positive outcome in the health system and that there will be more community health volunteers to be trained in the future.
Dr. Nosa Orobaton is a great doctor originally from Nigeria. He has worked all over the globe in leadership capacities at the WHO. Many many thanks to him for leading a team of 150 people to implement and scale a maternal child health and family planning program in two states in Northern Nigeria with USAID funding.He is working very hard on strategies to deliver proven, scalable interventions to those in need.